Vortioxetine Shows Potential in Glioblastoma Treatment, Clinical Trials Planned
ETH Zurich researchers have identified vortioxetine, an FDA-approved antidepressant, as a promising candidate in the fight against glioblastoma, a highly aggressive and often fatal form of brain cancer. In laboratory studies, vortioxetine was shown to effectively target glioblastoma cells, opening the door to potential repurposing of the drug in clinical cancer treatments. The results, recently published in Nature Medicine, emerged from a large-scale drug screening led by Professor Berend Snijder at ETH Zurich.
Glioblastoma presents a major challenge for treatment due to its resistance to conventional therapies and the difficulty of delivering drugs across the blood-brain barrier.
Sohyon Lee, lead author of the study, employed an innovative screening platform called pharmacoscopy to evaluate over 130 drugs, including antidepressants, Parkinson’s medications, and antipsychotics, against tumor cells from 40 glioblastoma patients. Vortioxetine was one of the few substances that demonstrated high efficacy in the lab, primarily due to its ability to cross the blood-brain barrier and act on tumor cells.
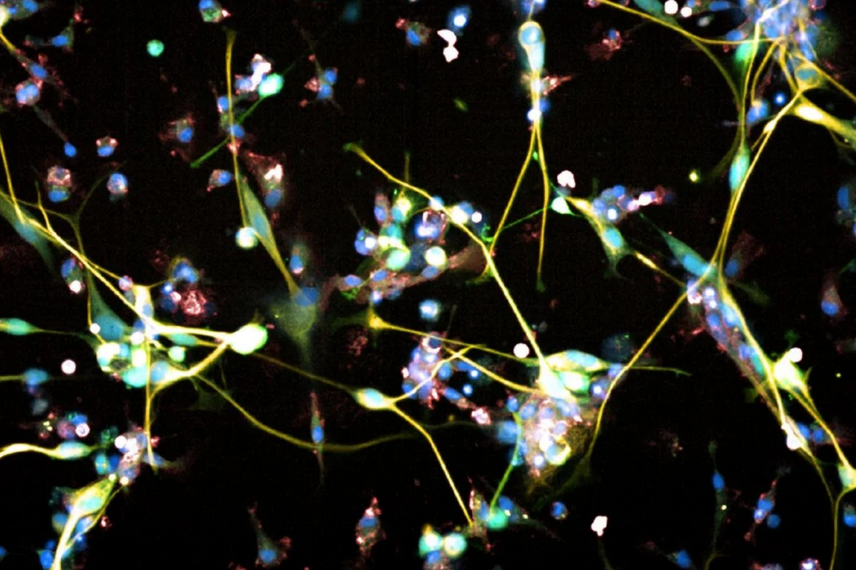
Illustration of deadly brain tumor cells, Glioblastoma. Credit: Sohyon Lee and Berend Snijeder / ETH Zurich
Pharmacoscopy, the platform developed by Snijder’s team at ETH Zurich, allows researchers to simultaneously test a wide array of drugs on living cancer cells. For this study, fresh cancer tissue samples from patients who had undergone surgery at University Hospital Zurich were processed and analyzed. Within days, the researchers identified which drugs were effective at targeting glioblastoma cells and which had no impact. Vortioxetine stood out as the most potent of the neuroactive drugs tested.
The discovery was surprising because antidepressants are not typically associated with cancer treatments. However, the research team found that vortioxetine triggered a signaling cascade important for neuronal progenitor cells, which also suppresses tumor cell division. This mechanism could explain why the drug was particularly effective at targeting glioblastoma cells.
Cellular Mechanisms Involved in Vortioxetine's Potential Treatment of Glioblastoma
Vortioxetine is hypothesized to combat glioblastoma by targeting neural-like pathways within tumor cells. Possible mechanisms include:
-
Serotonin Receptor Modulation: Vortioxetine interacts with serotonin receptors (particularly 5-HT receptors), influencing both neuronal and glioblastoma cell signaling. This modulation is thought to disrupt cell growth signals in cancer cells.
-
Calcium Signaling: The drug triggers a calcium influx in glioblastoma cells, mimicking neural activity. Calcium is vital in many cellular processes, including cell death pathways. Vortioxetine seems to hijack this process, increasing calcium oscillations in tumor cells, leading to their suppression.
-
AP-1/BTG2 Tumor Suppression Pathway: The drug activates the AP-1 transcription factors (e.g., JUN) and induces BTG2 expression, a tumor suppressor protein. This pathway is crucial for regulating cell proliferation, leading to reduced tumor growth and promoting cell death.
Michael Weller, Professor and Director of the Department of Neurology at University Hospital Zurich, highlighted vortioxetine’s potential benefits:
"The advantage of vortioxetine is that it is safe and very cost-effective. As the drug has already been approved, it doesn’t have to undergo a complex approval procedure and could soon supplement the standard therapy for this deadly brain tumor."
In collaboration with University Hospital Zurich, ETH Zurich researchers tested vortioxetine on mice implanted with glioblastoma. These preclinical trials showed that vortioxetine was not only effective in reducing tumor growth but also synergized with existing treatments like chemotherapy, improving overall efficacy.
Moving forward, two clinical trials are being planned. The first trial will explore the effectiveness of vortioxetine in combination with standard glioblastoma treatments—surgery, chemotherapy, and radiation. In the second trial, researchers aim to personalize treatment for individual patients using the pharmacoscopy platform to identify the most suitable drug combinations.
While the initial findings are promising, researchers caution against premature use of vortioxetine for glioblastoma patients. As Michael Weller emphasized:
“We don’t yet know whether the drug works in humans and what dose is required to combat the tumor, which is why clinical trials are necessary. Self-medicating would be an incalculable risk.”
Professor Berend Snijder also echoed a similar cautionary note:
"So far, it’s only been proven effective in cell cultures and in mice."
Despite these challenges, the discovery of vortioxetine’s effectiveness against glioblastoma cells represents a novel avenue for cancer research, focusing on the potential of neuroactive drugs to interact with brain tumors in ways previously not fully understood. The upcoming clinical trials will further determine whether this antidepressant can become part of the standard treatment for glioblastoma patients, offering new hope in a field where progress has been limited for decades.
The study highlights the benefits of drug repurposing, particularly for hard-to-treat cancers like glioblastoma. By leveraging existing, approved drugs that can cross the blood-brain barrier, researchers may accelerate the development of new therapies. If vortioxetine proves successful in clinical trials, it would be one of the first antidepressants to be repurposed for cancer treatment, offering a cost-effective and potentially life-saving option for glioblastoma patients.
The findings were published in Nature Medicine under the title “High-throughput identification of repurposable neuroactive drugs with potent anti-glioblastoma activity” on 20 September 2024. DOI: 10.1038/s41591-024-03224-y
Topics: Clinical Trials