Are We Keeping Up With Antimicrobial Resistance?
Antimicrobial resistance (AMR) poses a major threat to human health.
There were an estimated 4.95M deaths associated with bacterial AMR in 2019, including 1.27M deaths attributable to bacterial AMR.
Lower respiratory infections accounted for more than 1.5M deaths associated with resistance in 2019, making it the most burdensome infectious syndrome. The six leading pathogens for deaths associated with bacterial antimicrobial resistance are Escherichia coli, Staphylococcus aureus, Klebsiella pneumoniae, Streptococcus pneumoniae, Acinetobacter baumannii, and Pseudomonas aeruginosa.
Antibiotic resistance remains a public health crisis, and novel antibiotic drug discovery and development is imperative to outpace the ability of bacteria to develop resistance.
Only 17 new systemic antibiotics and 1 related biologic have been approved by the FDA since 2010. Among these drugs, 14 were approved for common bacterial infections, 1 was approved for Clostridioides difficile infection (CDI), 1 was licensed to prevent CDI recurrence, and 2 were approved for drug-resistant tuberculosis.
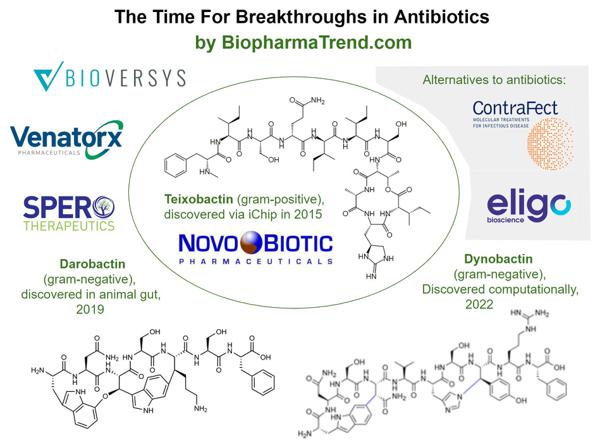
Unfortunately, the majority of these new drugs represent modifications to existing chemical structures rather than new drug classes.
In contrast to the Gram-positive field, where a variety of treatment options are available, the resistance situation in infections caused by Gram-negative bacteria is dramatic. Pan-resistant Gram-negative enterobacteriaceae or non-fermenters have only increased lately.
The number of new antibiotics and their indications are not keeping up with resistance and the needs of the patients.
Welcome any and all ideas and strategies from my network, please comment in thread, to combat antimicrobial resistance? We can do this together.
Topics: Bioeconomy & Society